- Home
- Products
- Pathway
- Support
- Contact Us

Renin-angiotensin system
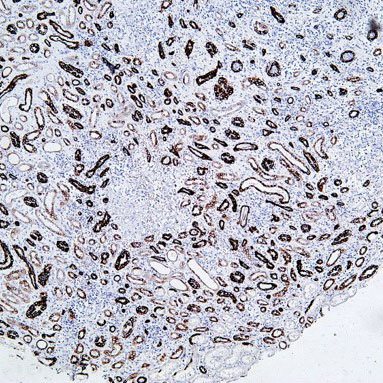
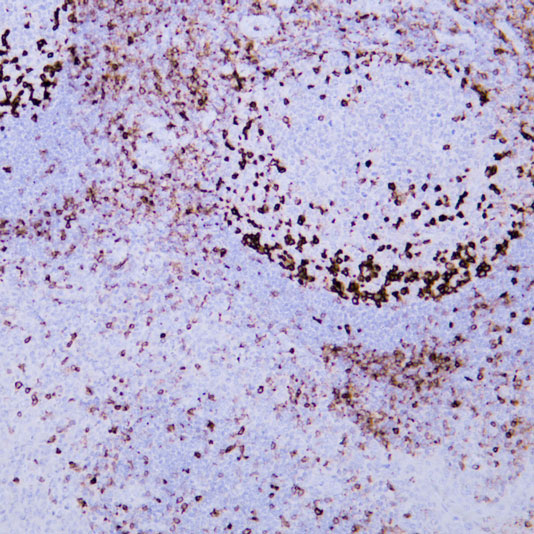
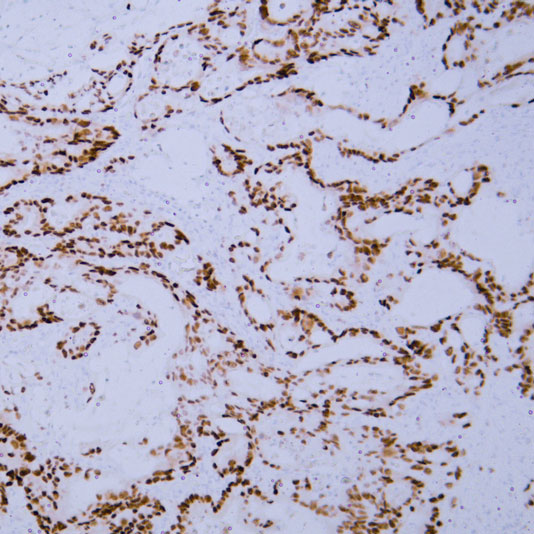
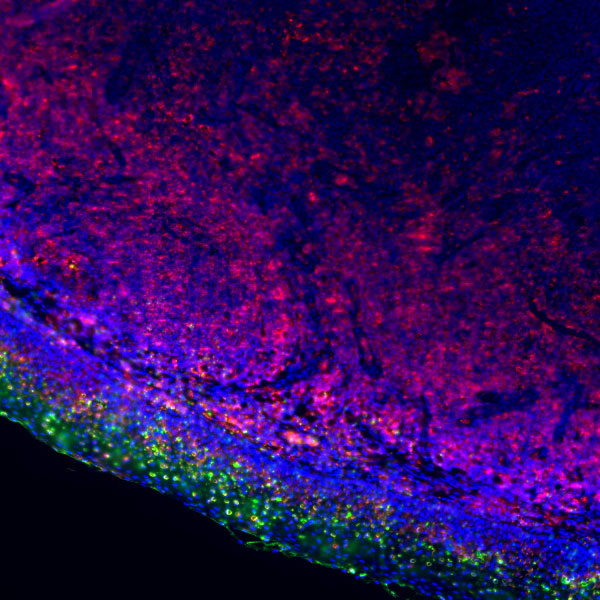
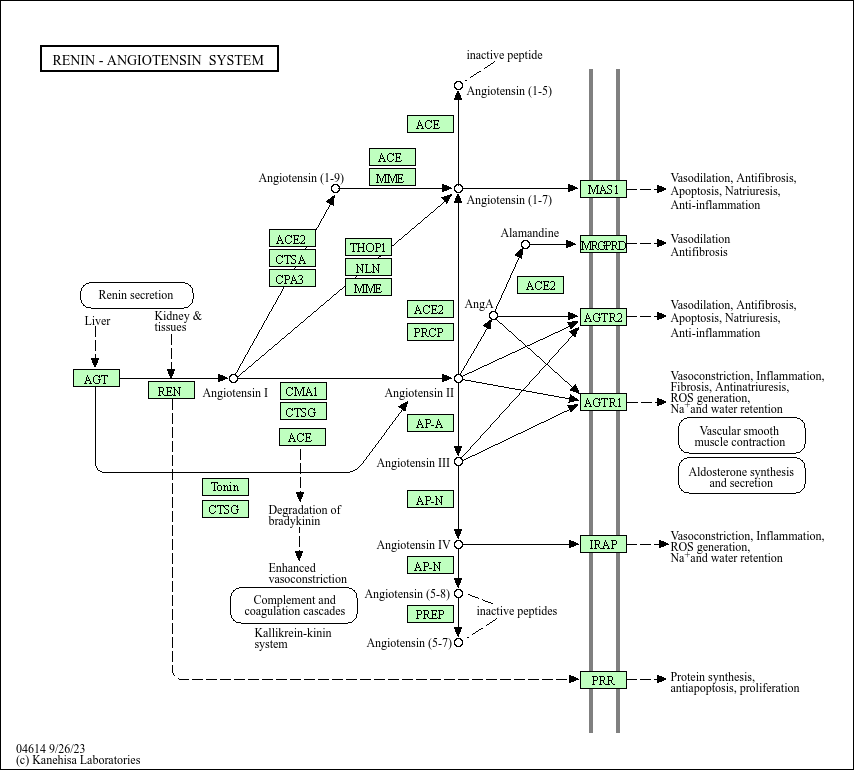
Core of basic research: Deciphers the molecular mechanism by which the RAAS regulates blood pressure, water-sodium balance, and vascular remodeling, a key pathway for cardiovascular homeostasis. Decreased blood pressure, reduced blood volume, or insufficient renal blood flow stimulates juxtaglomerular cells to secrete renin, which hydrolyzes liver-synthesized angiotensinogen into angiotensin I (Ang I). Ang I is hydrolyzed by angiotensin-converting enzyme (ACE) in the pulmonary circulation to form the core effector molecule angiotensin II (Ang II). Ang II binds to AT1R on target cells (vascular smooth muscle cells, adrenal zona glomerulosa cells, renal tubular epithelial cells), activating downstream signals: in vascular smooth muscle cells, the PLC-γ-PKC pathway induces vasoconstriction to increase blood pressure; in adrenal zona glomerulosa cells, it promotes aldosterone secretion to enhance renal sodium reabsorption; in the liver and kidneys, it promotes water-sodium retention and activates vascular remodeling-related genes. Additionally, Ang 1-7 (a product of Ang II hydrolysis by ACE2) binds to the Mas receptor, antagonizing Ang II-induced vasoconstriction to maintain pathway balance. Research focuses on the regulatory mechanism of renin secretion, the balancing role of ACE/ACE2, Ang II-AT1R axis signal transduction, pathway overactivation in hypertension, heart failure, and kidney diseases, and the therapeutic mechanisms of RAAS inhibitors (ACEI, ARB, renin inhibitors).
Core key proteins: Renin, angiotensinogen, Ang I/Ang II/Ang 1-7 (angiotensin family), ACE (angiotensin-converting enzyme), ACE2 (angiotensin-converting enzyme 2), AT1R/AT2R (Ang II receptors), Mas receptor (Ang 1-7 receptor), PLC-γ (phospholipase C-γ), PKC (protein kinase C), PI3K/Akt (core signal pathway), aldosterone, vascular smooth muscle cells, renal juxtaglomerular cells, adrenal zona glomerulosa cells.
Core key proteins: Renin, angiotensinogen, Ang I/Ang II/Ang 1-7 (angiotensin family), ACE (angiotensin-converting enzyme), ACE2 (angiotensin-converting enzyme 2), AT1R/AT2R (Ang II receptors), Mas receptor (Ang 1-7 receptor), PLC-γ (phospholipase C-γ), PKC (protein kinase C), PI3K/Akt (core signal pathway), aldosterone, vascular smooth muscle cells, renal juxtaglomerular cells, adrenal zona glomerulosa cells.
Product list
-
{{item.title}}{{item.react}}{{item.applicat}}
Product list
Product name
Reactivity
Application
Related Resource Links
Related Promotional Journal Downloads

Explore Our Recommended Popular Products
More products
30,000+ high- quality products available online
Primary Antibodies, Secondary Antibodies, mIHC Kits, ELISA Kits, Proteins, Molecular Biology Products,Cell Lines,Reagents ...
Contact Us